Cartilage Cultures Used For Knee Resurfacing
By David Dominguez, MD // February 3, 2014
FIRST CHOICE MEDICAL GROUP
BREVARD COUNTY • MELBOURNE, FLORIDA – Articular cartilage (AC) is the smooth, white tissue that covers the ends of bones where they come together to form joints.
 Healthy cartilage in our joints makes it easier to move. It allows the bones to glide over each other with very little friction.
Healthy cartilage in our joints makes it easier to move. It allows the bones to glide over each other with very little friction.
AC can be damaged by injury or normal wear and tear. Because cartilage does not heal itself well, doctors have developed surgical techniques to stimulate the growth of new cartilage. Restoring AC can relieve pain and allow better function, and most importantly, it can delay or prevent the onset of arthritis.
GOAL: STIMULATE NEW CARTILAGE GROWTH
The main component of the joint surface is a special tissue called hyaline cartilage. When it is damaged, the joint surface may no longer be smooth, which results in pain when the ends of the associated bones move over the damaged joint surfaces.

Damaged cartilage can also lead to arthritis in the joint. The goal of cartilage restoration procedures is the stimulation of new hyaline cartilage growth.
Abrasion, drilling and microfracture are techniques that have been used in the past in an attempt to repair articular cartilage lesions. However, these techniques were unable to recreate the normal characteristics of hyaline cartilage and resulted in the formation of fibrocartilage instead. Fibrocartilage is inferior to hyaline cartilage because it can degenerate over time resulting in short-term, temporary relief of symptoms, but ultimate early breakdown, leading to recurrence of symptoms and an increase in size of the cartilaginous defect, thus requiring further knee surgery.
AUTOLOGOUS CHONDROCYTE IMPLANTATION
Dr. Lars Peterson and colleagues developed autologous chondrocyte implantation (ACI) in Sweden during the 1980’s. It was developed to delay the onset of osteoarthritis by allowing regeneration of “hyaline like” cartilage.

Since its first introduction in Sweden, the FDA has approved the use of Carticel (autologous cultured chondrocytes) for the repair of symptomatic cartilaginous defects of the knee caused by acute or repetitive trauma in patients who have had an inadequate response to a prior arthroscopic or other surgical repair procedure.
ACI has been found to be beneficial for cartilage injuries greater than 2 to 3 square centimeters andis currently being used to treat cartilaginous injuries of the weight-bearing surfaces of the knee such as the femoral condyle, trochlea, patella and tibial plateau.
ACI INVOLVES A TWO STEP PROCESS
The ACI technique involves two separate surgical procedures: arthroscopy followed by an arthrotomy. The first procedure is a minimally invasive arthroscopic assessment of the knee joint performed as an outpatient. The area of defect is measured and articular cartilage is harvested from a non-weight-bearing surface for cartilage cell culturing. The biopsy is usually taken from the superior medial edge of the trochlea or the lateral aspect of the intercondylar notch if there is an overhanging patellar facet on the medial side. The cartilage biopsy is then cryo-preserved until the date of surgery is scheduled. At that time, it is thawed and cultured to the appropriate number of cell vials necessary for surgery.
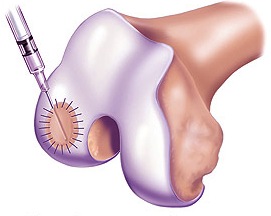
The second procedure is open ACI surgery performed at least 3-5 weeks after the biopsy is taken. The cartilage defect is debrided back to the subchondral bone with a rim of healthy cartilage. A template of the defect is made and a synthetic collagen patch is microsutured to the margins of the cartilage defect.
The cultured cartilage cells are then injected under the patch, which is subsequently sutured shut and sealed with fibrin glue. The joint is then closed and the procedure is complete. The injected cells must grow inside the joint to form a hard cartilage tissue, generally a 9-12 month process, and will continue to mature until up to 24 months.
REHAB IS CRITICAL TO SUCCESSFUL ACI
Rehabilitation after ACI is individualized based on the size, depth and location of the lesion, repair tissue maturation, as well as the condition of the surrounding articular cartilage. The goal of rehabilitation is to protect the graft while promoting maturation of the newly implanted chondrocytes through a program that focuses on regaining full range of motion (ROM), progressive weight bearing, lower extremity strengthening, flexibility and proprioceptive training.

Care must be taken to avoid compressive loading or shearing of the graft. Progression of rehabilitation is based on the three stages of healing–proliferation, transition, and remodeling/maturation.
Good outcomes have been reported in patients at 2 to 9 year follow-ups. ACI of isolated femoral condyle defects were found to be highly effective in relieving symptoms and restoring knee function. Most patients in this group returned to athletic activities in 12 to 18 months. Overall, ACI produces a durable and effective repair for as long as 9 years for full thickness cartilage lesions.
ABOUT THE AUTHOR

Dr. David Dominguez is a native of Melbourne, Florida. He is an Orthopedic surgeon fellowship trained in Sports Medicine and a member of the First Choice Medical Group. He is the only physician in Brevard County (and one of only ten in the State of Florida) trained to conduct cartilage preservation and restoration procedures; and is the only Orthopedic surgeon in the County qualified to perform Autologous Cartilage Implantation procedures for the treatment of cartilage defects of the knee. A graduate of Duke University Medical School, he is currently involved in cutting edge ACL surgery techniques, and has published research in hip replacement surgery and cervical spine injuries.